Optimal gut health stops the spread of food poisoning bacteria

Approximately 90% of all reported cases of foodborne illness are caused by Salmonella and Campylobacter, 2 families of bacteria that have been shown to have high levels of antimicrobial resistance. Ensuring gut health can stop food poisoning bacteria in its tracks.
Nearly 600 million people worldwide fall ill every year from eating contaminated food, according to the World Health Organization. Bacterial food infections – or food poisoning – are a major food safety issue and public health concern in both industrialised and developing countries.
From 2005 to the latest report in 2020, campylobacteriosis remained the most frequently reported zoonosis in humans. It is estimated that Campylobacter causes 1.5 million illnesses a year in the US alone. Studies into the source of Campylobacter infection in humans have associated it with contaminated poultry products which are believed to be a large reservoir for the pathogen. The organs of an animal, such as the intestines and liver, can contain Campylobacter and contaminate other edible parts of the animal at slaughter.
The UK Food Standards Agency in 2017 reported that 56% of chicken neck skin samples were contaminated with Campylobacter spp., 7% of which had levels of over 1,000 colony-forming units (CFUs) per gramme of chicken skin. The main route of Campylobacter transmission is commonly thought to be foodborne via eating raw or undercooked meat and meat products.
After campylobacteriosis, salmonellosis is the second-most frequently reported foodborne gastrointestinal infection in humans. The US Centers for Disease Control and Prevention estimates that 1.35 million infections each year in the US are caused by Salmonella, resulting in the deaths of 420 people.
Like Campylobacter, Salmonella causes diarrhoea, fever and stomach cramps. The main way Salmonella is transmitted to humans is through eating food contaminated with infected animal faeces. Eggs and egg products are one of the most common vehicles in foodborne salmonellosis outbreaks. Of the top 5 Salmonella strains responsible for human infections, 4 are known to have poultry – both broilers and layers – as their main source.
It is, therefore, critical that Salmonella is controlled in poultry to stop the spread of the bacteria to the human population. The best ways to decrease Salmonella infections from poultry include educating the public about best practices for raw meat handling and the importance of cooking meat thoroughly, improving slaughter hygiene and technology in processing plants to reduce contamination, and controlling infections in the poultry themselves.
Diversity protects against pathogen colonisation
Controlling both Campylobacter and Salmonella in poultry can be achieved through very high levels of biosecurity. However, this level of biosecurity is not feasible for most broiler farms. Therefore, a holistic approach is needed to reduce the levels of Campylobacter and Salmonella in poultry, part of which should include increasing the diversity of the gut microbiome, as it has been linked with enhanced resistance to pathogen colonisation.
Actigen, Alltech’s proprietary yeast mannan-rich fraction (MRF), is a unique, second-generation bioactive product derived from Saccharomyces cerevisiae. MRF has been studied for its ability to promote microbiota diversity and alter the overall composition of the bacterial community, helping to support the resilience of the gut against foodborne pathogens such as Salmonella and Campylobacter.
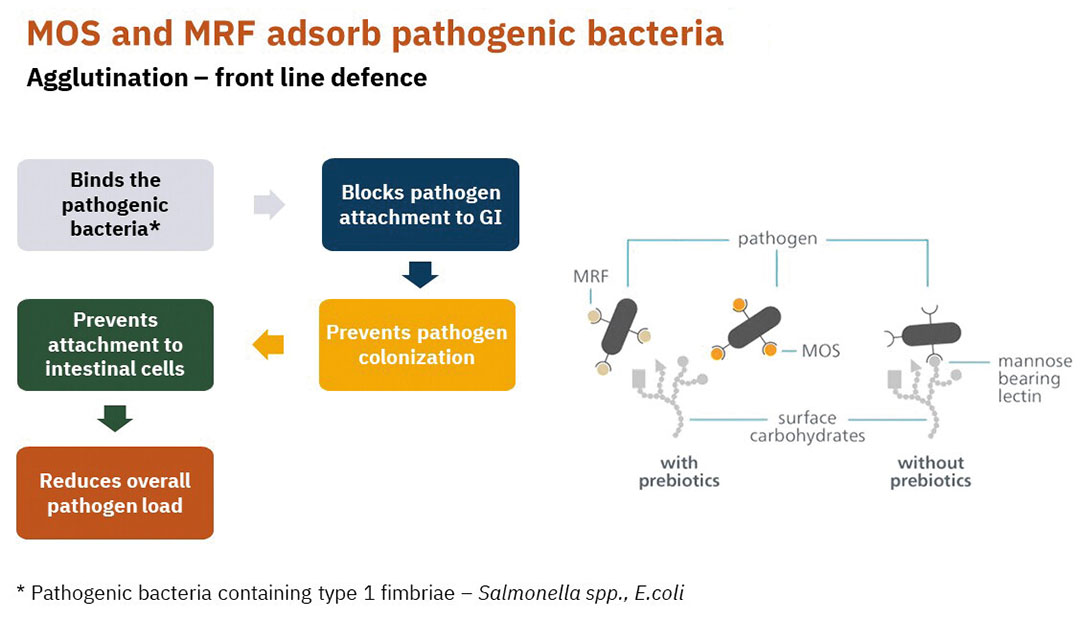
Research by Corrigan showed that MRF supplementation in the diet can significantly reduce Campylobacter colonisation levels in the broiler caecum and increase weight gain. MRF not only alters the microbiome of the gut but also agglutinates or binds Salmonella. Girgis’ study reported that MRF supplementation in layer diets significantly reduced both the prevalence of Salmonella in ovary tissue and its concentration in the caeca, making MRF supplementation a useful strategy for reducing the risk of eggshell contamination.
For Salmonella to colonise and infect the gut, it must first attach to mannose receptors via type 1 fimbriae. MRF can adhere to Salmonella, stopping it from attaching to and therefore colonising the gut. This makes MRF a great tool against Salmonella, because it has been shown to adhere to a wide range of Salmonella isolates. Salmonella controls need to be broad-spectrum because the nature and prevalence of Salmonella isolates is variable and isolates also change over time.
Foodborne illnesses often caused by antimicrobial resistance
An additional concern for food safety is the level of antimicrobial resistance harboured by the bacteria that cause foodborne illnesses. Antimicrobial resistance is a food safety issue because antimicrobial-resistant bacteria can transfer from animals to humans through the food chain. In the US, more than 2.8 million people every year become ill with antibiotic-resistant infections, resulting in 35,000 deaths. The burden on economies and health systems is considerable because antimicrobial resistance can lead to extended hospital stays, as well as more costly and intensive care.
Ampicillin, sulfamethoxazole and tetracycline have been used extensively in animal production as antibiotics, but these medicines are also important in the fight against bacterial infections in humans. In 2020, the overall resistance in Salmonella spp. found in broiler and turkey carcases to ampicillin, sulfamethoxazole and tetracycline were moderate to very high, reaching over 50% in some cases.
The increasing awareness and pressure surrounding antimicrobial resistance and the effects of using antibiotics in animal feed have led many countries to ban the use of antibiotic growth promoters in animal feeds. However, these bans are not enough to stop the greater emergence of antimicrobial resistance. It is a persistent issue, and rates of resistance are still high despite restrictions on antibiotic use. Because pathogens harbour resistant genes, it is critical to find ways to reduce resistance and increase bacterial sensitivity to antibiotics.
A 2017 study looking at the effects of feeding MRF reported that resistant organisms became more sensitive to antibiotics in the presence of MRF. Smith observed that Salmonella-carrying plasmids that conferred antibiotic resistance had decreased growth when MRF was present. Smith went on to report that the metabolism and growth of resistant E. coli changed when grown in the presence of MRF, resulting in an increased sensitivity to antibiotics. This increased effectiveness of the antibiotic used with MRF could result in a reduction in the level of antibiotic-resistant organisms in the bird and the environment, as well as the development of a diverse and more balanced microbiome.
Developing a robust, holistic approach to increasing food safety in poultry production is vital and should incorporate supporting the diversity of the bird’s gut microbiome to enhance resistance to pathogen colonisation and reduce the load of these bacteria in the bird. MRF can serve as an important tool in this approach, helping to improve resilience, as well as reduce antibiotic use and antimicrobial resistance.
References are available on request.
 Beheer
Beheer








 WP Admin
WP Admin  Bewerk bericht
Bewerk bericht